
Topical application of beneficial lactobacilli and potentially other ‘live biotherapeutic products’ (LBPs) show great potential as an alternative strategy to tackle skin care problems related to disturbance of the skin microbiome, providing alternatives to the overuse of antibiotics in skin care.
We caught up with Dr Ingmar Claes, CSO of YUN, a Belgian biotech company spun-out from the University of Antwerp to learn more about how they are developing LBPs to treat skin conditions.
MT: Words like “Balance” or “Dysbiosis” come up a lot when talking about the microbiome, but are hard to scientifically define – Can we talk accurately about Balance/ Dysbiosis when it comes to the skin?
Ingmar: The human skin functions as a protective layer against external factors and its most outer layer is formed of a multitude of micro-organisms, which means we can consider the skin microbiome our first line of defence. These bacterial and fungal species protect us from and compete with transient bacteria and other ‘invaders’ that could potentially harm us or infect us. As in nutrition and immunology, a healthy state is linked with a balanced microbiome. Even though defining ‘balanced’ is not straightforward, based on current knowledge, this balance is dependent on multiple factors, such as genetic, nutritional and environmental factors. Specifically for the skin microbiome, antibacterial ingredients formulated in skin care products, like soaps, creams, lotions, and shampoos can clearly impact the skin microbiome and disrupt this subtle balance, which develops from birth through to adulthood. Overgrowth of certain ‘bad’ bacteria, (‘pathogens’ or ‘pathobionts’) can then be linked to certain skin conditions and even infections. While dermatologists often try to treat such ‘dysbiosis’ with the use of antiseptics, antibiotics or antimycotics, we know that they are not always efficient and/ or sustainable solutions.
While there has been much debate on what constitutes a healthy microbiome, it is clear that it is all a matter of balance. Differences in the skin microbiome composition, either in diversity (alpha and beta diversity between body sites) and in the specific taxonomics strains present exist between individuals and skin locations. However, we now know which typical genera are present on the human skin based on the body site and whether it is dry, moist or sebaceous. Taking acne vulgaris as an example, it is specific Cutibacterium spp. (formerly known as Propionibacterium acnes) and also Staphylococci that play an important role in the pathophysiology of acne, the induction of inflammation and the formation of papules and pustules, i.e. ‘pimples’.
So can you speak of ‘dysbiosis’? Yes, excess sebum production and clogging of the pores alters the micro-environment and favours certain ‘pathobionts’. While these micro-organisms are also present on healthy skin , these shifts disturb the skin microbiome balance and result in a state of ‘dysbiosis’.
MT: How did YUN develop its science and come into formation?
Ingmar: Taking the learnings from the use of lactobacilli for gastrointestinal application and knowing that lactobacilli are the first bacteria we encounter as babies after a vaginal delivery, YUN’s research started focussing on the potential of using lactobacilli to tackle skin disorders with a first clear focus on acne vulgaris. With the research’s origin on ‘probiotic lactobacilli’ starting at the KU Leuven at the Centre of Microbial and Plant Genetics (prof. Jos Vanderleyden), the research on beneficial lactobacilli for topical application moved together with prof. Sarah Lebeer, currently President of YUN’s Scientific Advisory Board, to the University of Antwerp. Envisioning the potential of this research, YUN’s CEO Tom Verlinden, a pharmacist by training, started a collaboration with the University and established the company in 2014. After obtaining grants from the Flemish Government (VLAIO), the first products with ‘live’ lactobacilli entered the market April 2017. Besides the introduction of products with ‘live’ bacteria, a ‘microbiome-safe’ range was created. All formulations within this general skin care range were specifically developed to take care of the fine balance of the skin microbiome.
MT: A major problem with using probiotics as therapeutics seems to be keeping the ‘live’ bacteria, ‘alive,’ especially when passing through the Gastrointestinal Tract. Does treating skin conditions with probiotics also pose the same problem? How is YUN tackling this?
Ingmar: Both for gastrointestinal as for skin application, the challenge is to get the bacteria to the specific site of action ‘alive’ . While oral probiotics have to face the harsh conditions found in the stomach (low pH and enzymes) and the duodenum (bile salts), skin LBP’s need to face the stress conditions linked to the skin (low moisture, low nutrients, skin immunity, endogenous skin bacteria,…). On top of this, a major challenge to develop ‘live’ therapeutic bacteria for skin applications is linked to patient acceptance and compliance. So the final product should be pleasant to apply on the skin, while being compatible with ‘live’ bacteria. This means that in contrast with oral probiotics where a capsule with lyophilized powder can be used, the development of skin formulations containing water (creams, soaps, …) is very challenging.
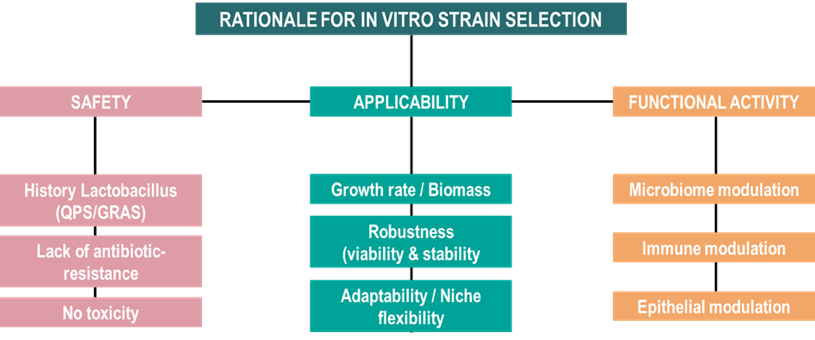
Moreover the question rises ‘which strains to select for specific skin applications’? Since live lactic acid bacteria are the first dominating our skin from a vaginal delivery to train our immune system, we believe in the safety and potential of these microbes to be used as therapeutics. We set up a rational selection/screening process (figure 1) to find the right stains of lactobacilli to improve acne symptoms.
After the in vitro selection of the specific Lactobacillus strains, the main hurdle was indeed keeping the bacteria alive up to a sufficient dosage to still observe the beneficial effect, as the multifactorial action of the beneficial lactobacilli requires viability and metabolic activity of the strains in situ. As this bottleneck was pinpointed in early stages of the R&D project, the collaboration with the lab of Pharmaceutical Technology and Biopharmacy (prof. Filip Kiekens and current R&D Manager Tim Henkens) was essential in the development of a new patented encapsulation technology compatible with water-containing products, like creams. This encapsulation technology opens up opportunities for multiple application of ‘live biotherapeutic products’ and multiple other fields outside skin care, to help keep the live bacteria live.
MT: Finally, you mentioned how you rationally screened and encapsulated your selected strains in the lab, but what about applying your product to patients? Have you seen results in humans?
Ingmar: YUN’s product for acne with the encapsulation technology was clinically evaluated in a clinical trial in collaboration with prof. Julien Lambert (MD) (University Hospital of Antwerp). The proof-of-concept trial demonstrated a significant reduction in comedonal and inflammatory lesion after 4 weeks of twice daily use of the topical probiotic product, in patients with mild to moderate acne. Moreover, there was a post market follow-up study conducted, with more than 6% of Belgian dermatologists confirming the results from the clinical trial and proving the potential of live biotherapeutic products in skin care.
This demonstrates that while patients and dermatologists are struggling to find the best treatment option for acne vulgaris in terms of benefit/efficacy and risk/side effects, topical probiotherapy (i.e. live bacteria in sufficient amount to confer skin health benefits) offers an alternative to reduce topical and oral antibiotic use in trying to treat acne vulgaris. For more severe cases of acne vulgaris, the product has no contra-indication to be used in combination with oral antibiotics as well as retinoids, where it can act synergistically from the outside.

