The Jackson Laboratory (JAX), a nonprofit biomedical research institution, and Azitra, Inc., a company developing microbiome-based therapeutics to treat skin diseases and conditions, have been awarded a $500,000 grant from the Department of Defense (DoD).
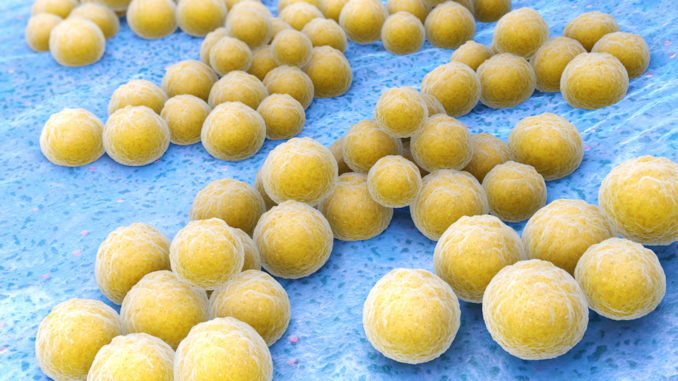
The goal of the program is to identify bioactive compounds produced by Staphylococcus epidermidis (S. epidermidis) that can inhibit Staphylococcus aureus (S. aureus) and ultimately treat skin infections.
S. aureus is the predominant organism causing many skin problems including “staph” infections. S. epidermidis is a natural commensal organism that lives on the skin of humans and is known to produce bioactive compounds that inhibit S. aureus. The research conducted under this program will explore the use of potent antimicrobials derived from S. epidermidis that may be able to act as natural defense mechanisms against skin infections. By utilizing different growth mechanisms and genetic tools, JAX and Azitra will evaluate the ability of diverse S. epidermidis isolates to inhibit S. aureus and characterize the native antibiotics produced by S. epidermidis. Building on this initial work, the JAX/Azitra team will investigate both the bioactive compounds and also engineer strains of S. epidermidis to produce therapeutic levels of those bioactives that can be applied to the skin. Julia Oh, Ph.D., a skin microbiome expert and assistant professor at JAX, will serve as the JAX principal investigator for this research, and Azitra’s Founder and Chief Scientific Officer, Travis Whitfill, MPH, will serve as Azitra’s principal investigator under this grant.
“The microbiome offers a new approach to understanding skin disease and developing new strategies to improve patients’ lives,” said Oh. “This research will extend our understanding of how the bacteria making up the microbiome compete and has the potential to generate new tools to combat challenges such as staph infections.”
Antiobiotic resistance is a growing crisis, and the United Nations General Assembly in September 2016 met to devise strategies to combat this rising crisis1. A project commissioned by the British government—the Review of Antimicrobial Resistance—found that by 2050, there could be as many as 100 million deaths per year and at least $100 trillion in sacrificed gross national product due to resistant bacterial infections2. In the United States alone, the CDC estimates that over two million illnesses caused by bacteria are resistant to at least some classes of antibiotics and of the two million antibiotic resistant illnesses, over 23,000 deaths occur each year3.
“We are very grateful to receive this funding to support research in an area that represents such a large and growing need,” said Whitfill. “Antibiotic resistance is a growing public health crisis, and the use of a new class of antimicrobials against MRSA has tremendous promise. If this work is successful, we are also looking at extending this platform beyond S. epidermidis and S. aureus as a broader tool for novel antibiotic discovery. We are very excited to begin this research with Dr. Oh’s team and JAX to develop a novel approach for preventative and acute treatment of MRSA and skin infections using Azitra’s microbe-based technology platform.”
The challenge posed by S. aureus infection of the skin is growing and the need for new bioactive compounds to address this problem is significant. This is especially true with the increasing rate of development of antibiotic resistance. Many strains of S. aureus have become resistant to traditional antibiotics; for example, methicillin-resistant S. aureus (MRSA), is a predominant cause of S. aureus infections in both the healthcare and community settings. MRSA is often implicated in acute bacterial skin and skin structure infections (ABSSSIs). These resistant strains are highly prevalent across the healthcare continuum and have been implicated as a cause of morbidity, mortality, and increasing healthcare costs. Current and new strategies to manage MRSA and S. aureus infections are limited to small molecules and the use and effectiveness of these antibiotics has been declining.
